Despite their best efforts and expert knowledge, it is impossible for radiologists to completely avoid misdiagnoses. However, as radiological findings often determine the course of subsequent treatment, incorrect or delayed diagnoses have the potential to cause great harm. In this article, we outline crucial liability issues and offer five strategies on how to keep the error rate in radiology as low as possible.
What counts as a misdiagnosis in radiology?
A misdiagnosis occurs when imaging exams – like X-rays, MRIs or CTs – are incorrectly evaluated. These boil down to three main types of error:
- Radiologists may miss pathological changes on x-rays, such as nodules or shadowing.
- Normal findings may be misinterpreted as being pathological (e.g., if the epiphyseal line on a child’s x-ray is mistaken for a fracture).
- Radiologists may recognize a pathologic change but misinterpret it (e.g., a carcinoma is mistaken for a harmless cyst not requiring treatment).
In a highly influential report, the US National Academy of Science, Engineering, and Medicine (NASEM) developed a broader definition of misdiagnosis. The report cites that a diagnostic error occurs when it fails to:
- (a) find an accurate and timely explanation for the patient’s health problems, or
- (b) communicate the diagnosis to the patient (in an understandable way).
With this patient-centered definition, NASEM has pointed out two further sore points in our healthcare system: Diagnoses can sometimes be made too late, or lack of communication between radiologists, physicians and patients can lead to subpar treatment results.
How likely is a misdiagnosis in radiology?
Conservative estimates show that the error rate in imaging exams average 3-5% – which means 40 million misdiagnoses occur every year worldwide. These error rates can vary considerably depending on the type of exam and the circumstances.
However, despite the extensive research available, it is difficult for methodology to determine the exact error rate in radiology exams. This is because X-ray, CT or MRI images often don’t allow for straightforward interpretations, which is why they are mainly used for preliminary diagnoses. Even if a suspected diagnosis turns out to be wrong in retrospect, this may not signal a “misdiagnosis” during the initial exam.
What should you do when accused of misdiagnosis?
If a patient believes they have been harmed due to a misdiagnosis, they can sue for damages and compensation for pain and suffering. The legal risk caused by misdiagnosis in radiology should not be underestimated: In the US, 2,441 radiologists faced legal action between 2015 and 2019 – mainly linked to breast cancer diagnoses. The average compensation payment was $551,295.
Unlike in many European countries, there is no general legal obligation in the US to have professional liability insurance – but this is highly recommended. Professional liability insurance covers justified claims for damages by patients, and also defends against any unjustified claims (passive legal protection). In most cases, insurance also covers the costs of medical reports. In the event of an accusation with grounds, the first step should be to contact your professional liability insurance to discuss what to do next.
Often, good communication with patients or their relatives can defuse a situation. But be careful: Patients have the right to be given a copy of their patient files at any time, and can ask for details about their diagnosis or treatment process. Liability insurance policies typically prohibit physicians from acknowledging fault. This means that their actions should be described as neutrally as possibly, without evaluation.
When are radiologists liable for a misdiagnosis?
Although misdiagnoses are a regular occurrence in radiology, it’s comparatively rare that they lead to actual convictions. This is because a misdiagnosis does not automatically establish medical liability. In almost all Western legal systems, the decisive factor is whether the physician can be charged with a breach of their duty of care.
This means that radiologists do not owe patients a correct diagnosis. Rather, they must offer treatment only in line with “lege artis”, meaning that it must satisfy the current standard of medical practice. If medical experts find that the diagnostic error was reasonable, then this usually does not lead to legal consequences.
A tricky legal question is: Who in the hierarchy is liable for a misdiagnosis? The radiologist or their employer as a legal entity? This often depends on the individual agreements set out in the employment contract. Employed physicians should therefore carefully check their employment contract and, if in doubt, seek legal advice. This also applies if professional liability insurance is already included in the contract. In such cases, it is vital to ask what the exact terms and conditions of this are, e.g., whether there is retroactive indemnity cover when the employee leaves the company.
Reducing error rates: 5 strategies for risk reduction
It’s impossible to fully prevent misdiagnosis in radiology. In fact, they occur regularly and predictably, and should not be judged as personal failures of individual experts. Instead, it is more effective to take a neutral and objective approach to better understand the reasons for misdiagnosis. Based on these reasons, strategies can be developed to reduce the risk. Here are 5 steps that radiology clinics can take to reduce their error rates:
1. Find system-related causes for misdiagnosis
A misdiagnosis is often caused by system-related factors that an individual physician has only limited control over. These systemic factors include staff shortages, high workloads, excessive duty hours, frequent distractions, lack of standardized processes, or unclear distribution of tasks and skill sets within a team. Though it may be difficult to make immediate changes to these challenging conditions, radiology clinics should be aware of these weak points and work out step-by-step solutions.
2. Optimize communication processes
Radiology clinics are complex organizations, making them particularly susceptible to communication issues. Important information can get lost, diagnoses are too late, or referral clinics and patients may not receive clear information. To solve these issues, standardized and optimized communication processes are key. This step can significantly help reduce rates of misdiagnosis in radiology. Critical tools here include multidisciplinary team meetings, case discussions, checklists, peer reviews, structured reports and electronic patient records.
3. Be aware of possible cognitive biases
On an individual level, making radiological diagnoses requires complex perceptual and thought processes – naturally, these are susceptible to interference. With added stress and time pressure, there is a latent risk of cognitive biases – which can cause misdiagnosis.
Some examples of cognitive biases are:
- Satisfaction of search: There is a tendency to prematurely stop the diagnostic process as soon as an abnormality has been detected – especially if this offers a plausible explanation for the patient’s complaints. A radiologist may then overlook additional shadowing at the edge of the scan, for example.
- Anchoring bias: The first available information is perceived to be more important and is (unconsciously) adhered to – even when later information contradicts it.
- Availability bias: When a certain clinical picture can be mentally recalled, it is considered more probable. For example, when a radiologist has made a diagnosis the day before, then sees a clinically-similar pattern, yesterday’s diagnosis will come to mind first.
- Attribution bias: Certain patient attributions (such as “alcoholic”, “depression-prone”, “obese”) can narrow the perspective and cause a physician to no longer judge a patient neutrally or objectively.
It’s not always possible to fully avoid cognitive bias, particularly when working under time pressure. However, understanding these biases can help professionals reflect on their own thought processes. There are also options for additional support tools, such as checklists, peer review systems or technological assistance systems.
4. Watch out for mental and visual fatigue
Mental and visual fatigue – not to be confused with cognitive bias – can also impair judgment and lead to misdiagnosis. Fatigue has physiological causes: Even if training can extend individual stress limits, the human brain is fundamentally incapable of concentrating for hours on end. The following strategies can help reduce the risk of fatigue:
- Schedule more challenging cases for the beginning of a shift
- Take short and structured breaks, or switch between different tasks
- Reduce disturbances and distractions as much as possible
- Optimize the workspace (ergonomics, lighting, etc.)
- Use technological assistance systems
5. Use modern medical technology to avoid misdiagnosis
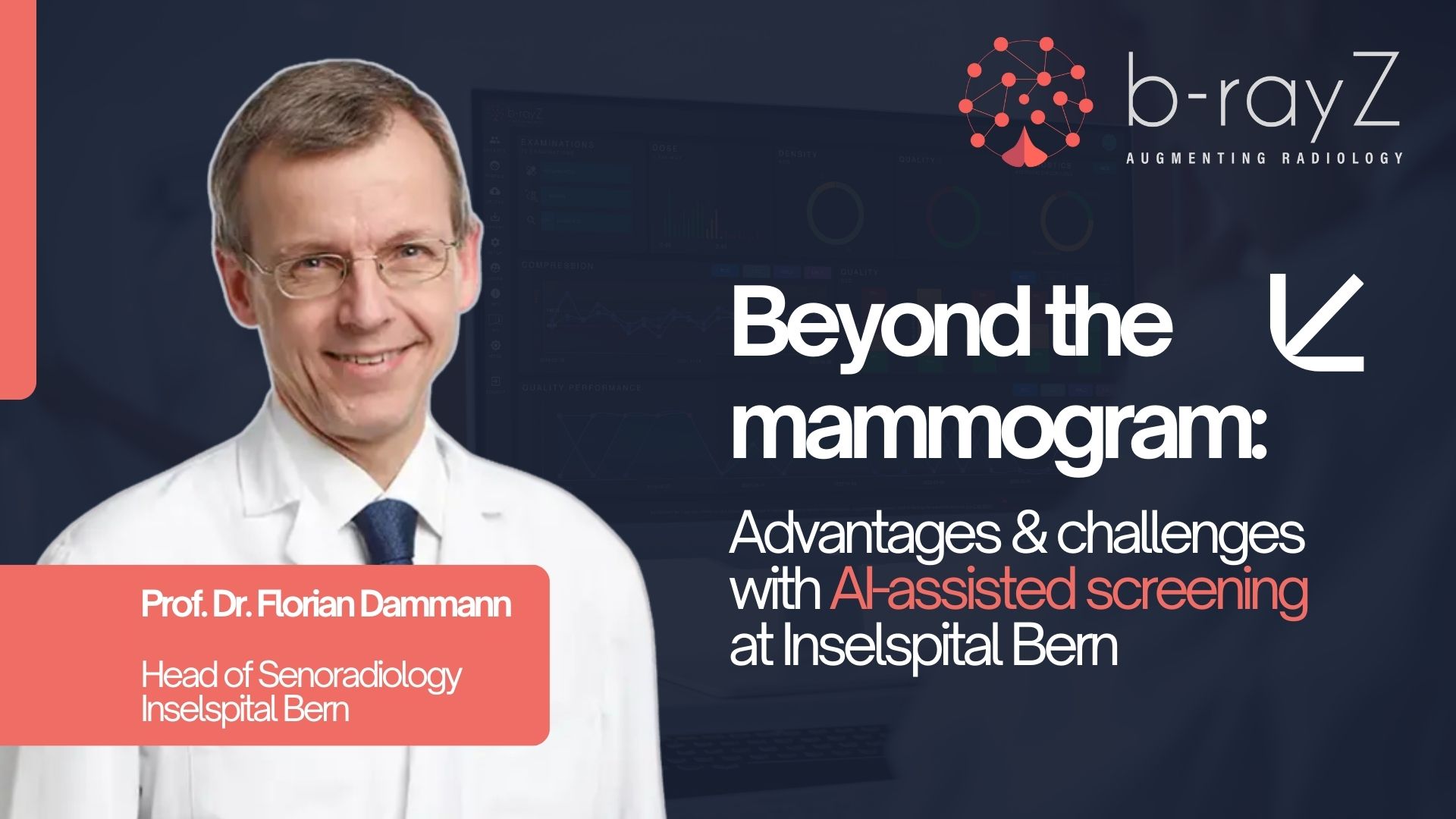
Innovative healthcare technologies can play a key role in reducing radiology error rates, ultimately increasing patient safety. One example is digital breast tomosynthesis: studies show that this offers higher specificity in comparison to conventional X-ray mammograms, which can help avoid false-positives.
Technological assistance systems, like those based on artificial intelligence, can be vital in compensating for “human” error sources, such as cognitive bias or fatigue. These solutions increase efficiency and patient safety in everyday clinical practice, reducing the risk of misdiagnosis.
Crucial: Keep an open and constructive approach to misdiagnosis
Misdiagnosis in radiology is caused by a complex interplay of systemic and individual factors. It’s impossible to completely avoid errors in everyday clinical practice, but it is possible to minimize them. To reduce error rates and liability risks, it’s important to understand the possible causes and to develop strategies to improve diagnostic decision-making processes. First and foremost, a neutral and constructive approach to errors is vital. After all, “blame and shame” mentalities, which pin the blame on individuals, are scientifically unjustified and don’t help reduce misdiagnoses.