Artificial intelligence (AI) in medicine: a subject that’s polarized the public and raises alarm as well as high expectations. However, our lives have already undergone unseen digital transformations in a host of different ways – not just through AI, but also Big Data. We speak to smart speakers and to our smartphones or receive personalized training tips from our fitness trackers. There’s barely a field that has a higher complexity and data-use than medicine – and that makes it a prime area for applying artificial intelligence. There are many myths circulating about the opportunities and risks of using AI in medicine – but these don’t always stand up to a reality check.
What is Artificial Intelligence (AI)?
It’s difficult to give an exact definition of artificial intelligence (AI) because science still can’t agree on a definition of human intelligence. In general, “AI” encompasses the ability of machines to carry out tasks and make decisions in a way that simulates human behavior.
AI doesn’t just refer to a single technology – there are many types of processes and methods. An exciting sub-sector is machine learning (ML). Here, basic data sets provide algorithms, laws and patterns that can be applied to unknown future situations. Another example is “deep learning”, which uses artificial neural networks made of many different layers.
What can AI do for medicine?
In recent decades, there’s been a digital revolution with its methods and technology transforming the medical field. We’re no longer waiting to develop X-ray images in a darkroom or counting cell cultures under a microscope. What was once a time-consuming manual job can now be done by a computer program. And these programs are much more efficient and reliable than people.
Today, medicine is facing another transformation through AI: 3D imaging, biometric data, genome sequences and more are all generating huge amounts of data. This data has a huge potential, but it can’t be fully exploited with conventional processing methods. This is where AI comes in – AI applications can effectively manage and analyze vast and complex data sets. Ideally, AI in medicine can generate new knowledge to improve medical care.
How is AI used in medicine?
There are so many diverse applications for AI in medicine. Some of these have already found a clinical use. These include fields such as:
Diagnostics
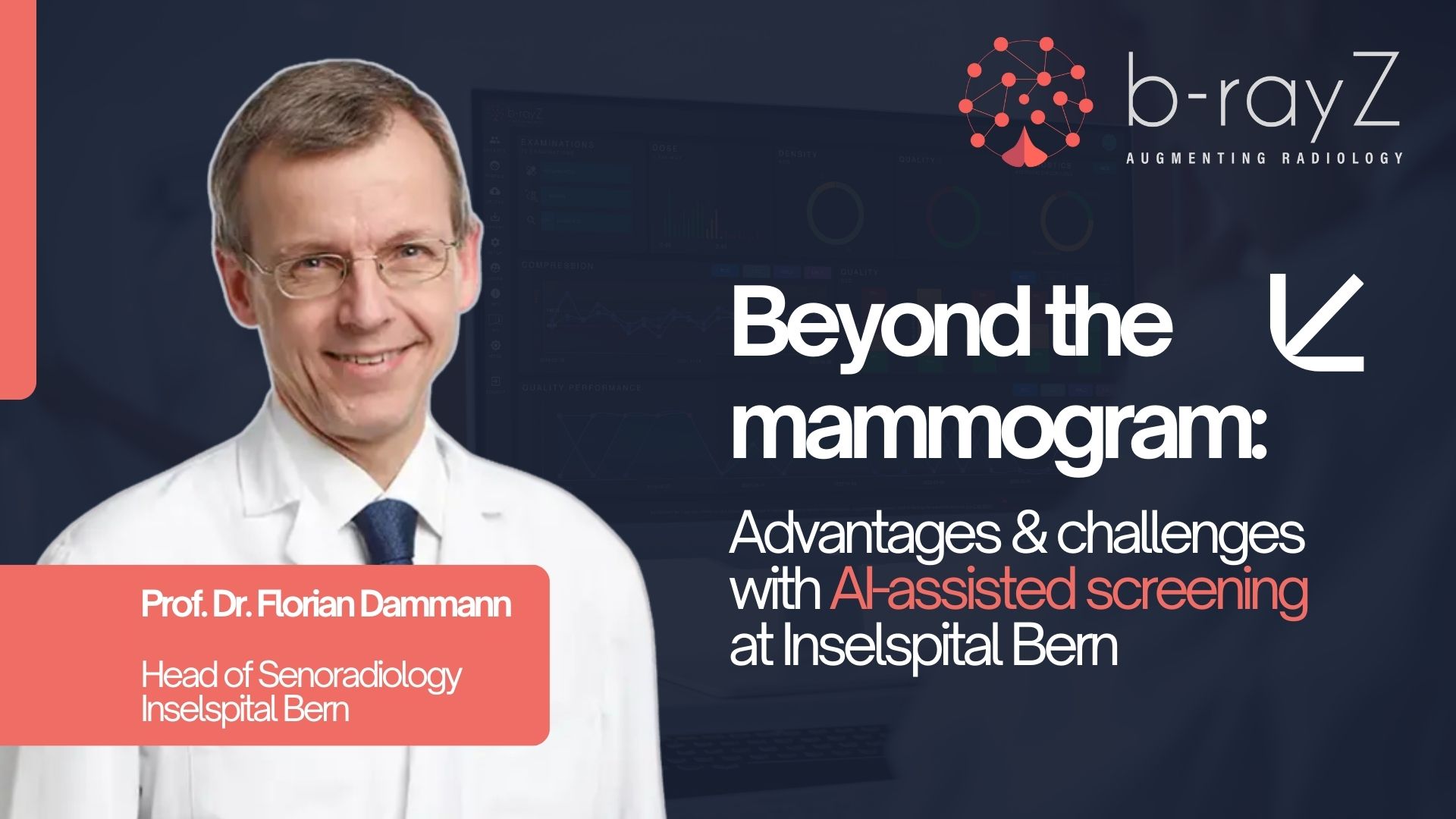
AI is especially valuable when used in the field of diagnostic imaging. As the basic data is already digital, by using deep learning, we can train AI systems to make independent diagnostic decisions. For example, AI is more reliable at detecting tuberculosis on chest X-ray images than an experienced radiologist. AI solutions can even determine bone age in pediatric radiology, improving accuracy and reducing the wait for a diagnosis.
Developing pharmaceuticals
Developing new drugs is time-consuming and expensive. Yet, AI can significantly speed up some of the steps required, such as:
- Identifying the right intervention targets at a molecular level
- Analyzing potential active ingredients through their biochemical properties
- Identifying and grouping suitable subjects in clinical studies
Tailoring treatments
Not all patients respond to drugs and treatments the same way. If the right data sets are available, AI systems can predict how a patient will respond to a specific treatment by comparing previous treatments and their results. In this way, AI in medicine can offer tailor-made therapies with better results and fewer side effects.
Improving early detection
An exciting potential of AI systems lies in personalized predictions. Different databases can be linked to identify individual health risks at earlier stages. With early diagnoses, people can plan and target pre-emptive treatment more effectively.
Easier genome analysis and editing
The use of AI in medicine can deepen our knowledge of human genome patterns, telling us who is more at risk of certain diseases. Links between genome patterns aren’t always straightforward and conventional statistical methods are pushed to their limits by the sheer amount of data.
AI can also improve the accuracy of genome editing using the CRISPR method. For example, AI algorithms can make it quick and simple to select suitable gene target regions.
Robot-assisted surgery
Intelligent surgical instruments coupled with high-resolution 3D cameras are already assisting in ORs today. Robotic or AI-supported systems can provide even gentler and more precise incisions, particularly for minimally invasive procedures.
Monitoring chronic diseases
Fitness trackers, which are essentially small portable computers with sensors, have long since been a part of everyday life. This form of AI in medicine offers an easier way to manage chronic diseases in the future. In the case of diabetes, for example, closed-loop systems are now readily available: these use a sensor to continuously measure a user’s glucose levels in their subcutaneous fatty tissue. They then automatically adjust the insulin dose via a pump.
Hospital data management
Most hospitals produce huge amounts of data every single day. AI can help manage this data in the most efficient way and make it available when and where it’s needed most.
What opportunities does AI offer in medicine?
We’ve already seen how effective AI in medicine can be in areas such as image interpretation or quantification of biomarkers, for example. AI can be especially useful for standardized tasks, that are time-consuming and monotonous. AI is much more efficient and often more reliable in such cases. Unlike human brains, AI systems will never get tired or make careless mistakes.
In all its applications, it’s crucial that AI in medicine is used ethically. That means that there has to be a rational way of understanding how the AI system makes decisions. After all, even artificial intelligence isn’t infallible. In medicine, wrong decisions can have serious consequences.
Myths about AI in medicine – So, what’s true?
Change often causes fear and skepticism for the public, giving rise to myths and conspiracy theories. Below, we’ve busted some of the most common myths on the use of AI in medicine.
Myth: AI will soon replace medical staff
Doubtless, AI will take over certain medical tasks that were previously carried out by people. However, medical professionals will never be replaced – instead, their areas of responsibility will change. In the future, medical facilities will need more specialists who can develop or operate AI systems. However, the human aspect of patient care is irreplaceable, and won’t be taken over by machines.
It’s crucial to remember that many medical and patient care sectors are already suffering from a significant labor shortage – and this will continue to worsen due to globally aging populations. Given these conditions, AI systems can offer vital support to maintain high-quality medical care.
Myth: AI is already making decisions in hospitals and other medical facilities
Right now, medical decisions in hospitals are and will probably continue to be made by trained experts. While AI systems can suggest possible diagnoses and treatments, these options are always double-checked by doctors who are familiar with the patient and the overall medical context.
Myth: AI in medicine could spin out of human control
AI may lead to unforeseen results that come as a surprise to its developers. However, it is impossible for it to get out of human control. Moreover, AI has no intentions or goals of its own. Important medical decisions in clinics will continue to be made exclusively by human experts, based on their knowledge and experience. AI in medicine is just another tool, among many others.
Myth: Only large clinics will be able to afford highly specialized medical AI solutions
Sophisticated AI systems enable clinics to offer medical services at the same or higher quality – with greater efficiency and fewer resources. In this way, AI systems can be of great help to smaller medical facilities, ensuring that they can compete with larger clinics.
Myth: AI is infallible
AI systems are only as good as the databases and algorithms that they’re based on. If these databases are biased or incomplete, then it’s possible for AI to draw the wrong conclusions. That’s why it’s crucial for trained experts to monitor how AI systems are applied. Ultimately, these human experts bear the responsibility for AI medical decisions.
On the other hand, AI in medicine can reduce common human errors: most often, these are mistakes and oversights caused by exhaustion. In addition, AI can help inexperienced doctors make diagnoses. Overall, applying AI in medicine can significantly increase the quality of care.
Myth: It’s impossible to know how AI systems make decisions
This may have been partly true in the early days of AI research. In particular, artificial neural networks often behaved in mysterious ways that developers couldn’t immediately understand. However, this isn’t at all true for modern, mature AI applications. These days, AI systems – especially those being used in medicine – are designed so that experts can understand exactly how solutions are found.
Myth: Using AI in medicine can lead to data protection leaks
Big Data – this is ultimately what has made the development and use of AI in medicine possible. Essentially, this involves sensitive personal information that is subject to specific data protection laws, such as the European General Data Protection Regulation (GDPR) or the US Healthcare Insurance Portability and Accountability Act (HIPAA). However, it’s possible to use this personal information in a data protection-compliant way to develop better AI systems.
When using AI in medicine, it’s the norm to receive explicit patient consent for data use. In the future, healthcare facilities using AI systems will have to be more vigilant around data security, as unauthorized access (e.g., cyber-attacks) can lead to breaches of data protection.
AI in medicine offers efficient and patient-centered care for the future
There are many myths about the use of AI in medicine, but these are the result of incorrect or outdated information – or unrealistic expectations. Artificial intelligence cannot replace the specialized knowledge and experience of medical experts. However, it has already proven to be a great tool for tackling time-consuming, routine tasks and for effectively analyzing large databases. This not only gives medical experts time for more important tasks, but AI can continue to ensure patient-centric, high-quality medical care now and in the future. The fact is that personal patient care, creative thinking and holistic understanding will firmly remain in the domain of human intelligence.