Mammograms are a core part of detecting breast cancer early, which can significantly improve a patient’s prognosis. But radiology centers that offer state-organized screening programs often face major challenges: correctly performing a diagnostic mammogram and generating a valid report requires profound specialty knowledge. At the same time, patients feel nervous and unsettled during breast exams, requiring a sensitive and empathetic bedside manner. The key here is to optimize and standardize workflows to ensure the highest quality medical care, and to provide women with a comfortable experience.
What are the benefits of diagnostic mammograms for early breast cancer detection?
A mammogram is an X-ray-based exam of the female breast that shows breast cancer (mammary carcinoma) or its precursors. Currently, it’s the only early detection method that has proven to reduce breast cancer-related mortality. As early as the 1980s, women taking part in organized screening programs benefited from a 20% risk reduction. A recent Swedish study estimates that patient mortality rate in breast cancer screening programs is reduced by 41%.
How are mammogram screening programs organized?
In Europe, the 1980s saw the introduction of nationwide mammogram screening programs in countries such as Sweden, Finland and the Netherlands. Now, state-organized screening programs are the norm in almost all EU countries, though these differ slightly in terms of the target population and screening intervals. The European Commission has set out firm guidelines on the quality requirements for breast cancer screening and diagnosis.
In the US, the Mammography Quality Standards Act (MQSA) sets the quality standards that healthcare facilities must offer as part of their mammogram screening for early breast cancer detection. These facilities must:
- Be certified by the FDA or an FDA-recognized accreditation body
- Undergo annual inspections
- Make sure their certification is accessible and visible to patients
Unlike in Europe, the US as yet has no legislated routine breast cancer screening program. Nevertheless, many women have access to free or low-cost diagnostic mammograms. For example, uninsured women can turn to the National Breast and Cervical Cancer Early Detection Program coordinated by the CDC (Centers for Disease Control and Prevention), which offers free diagnostic screening.
While European early-detection programs are mainly targeting women aged over 50 and take place at two-year intervals, US specialists recommend the first exam at 40, with only one-year intervals.
Early breast cancer detection through diagnostic mammograms: The optimal process
Step 1: A medical consultation (optional)
Before a mammogram, women are usually entitled to speak to their radiologist for informed consent. This consultation offers women the opportunity to ask questions and receive tailored advice, so they can make an informed decision. As trusted experts, gynecologists and general practitioners are also responsible for providing sufficient information on mammograms and recommending eligible women for screening programs.
In Germany, women first schedule a consultation appointment through their state’s central office (“Zentrale Stelle”). Women who don’t want a consultation can fill out a waiver to bring with them to their mammogram appointment.
The consultation should outline detailed information on the procedure, as well as all possible limitations of a diagnostic mammogram. Doctors should explain the best times for performing such a screening: For pre-menopausal women, mammograms are most effective in the first half of the menstrual cycle, as the breasts are softer in this phase. This makes the mammogram more comfortable for the patient, while also making the resulting images easier to evaluate. For post-menopausal women, the timing is irrelevant. If a woman presents symptoms, early breast cancer detection mammograms can be performed at any time.
Step 2: Scheduling an appointment
In Germany, mammogram appointments as part of early breast cancer detection screenings are organized by a central state office. When women contact their local radiology clinic directly to make or change an appointment, they’re usually referred to this central office.
In other countries, women can reach out to their health insurance via phone or online, to find out which local clinics offer diagnostic mammograms and how to register for them.
Step 3: Preparing for the exam
On the day of the exam, the patient should bring her insurance card to the appointment. She can fill out a medical history either at home or on site, where the reception staff can offer help.
Mammograms are carried out by a radiographer. Typically, this radiographer is the only medical professional the woman will interact with that day, so it’s crucial that they offer a good standard of care to make the examination as comfortable as possible.
Preparing for the exam includes these further steps:
- The radiographer asks the patient about any previous experiences with diagnostic mammograms, and any breast-related complaints. They will also answer any questions.
- They briefly explain the exam procedure to the patient. The radiographer should also explain why brief breast compression is necessary: Compression leads to better imaging quality as it reduces blurring and overlapping. It also reduces the radiation dose.
- On the day of the mammogram, the patient should refrain from using personal hygiene products like deodorants or body lotions in the breast and armpit area – doing so can lead to distorted images. Radiographers should check before the exam that no such hygiene products have been used.
- The patient then undresses her upper body and, if necessary, removes earrings or necklaces.
- Pregnancy should first be ruled out in women of childbearing age. Next, shielding wraps or aprons are put on for protection.
Step 4: Performing the mammogram
Usually, two standard images are taken of each breast:
- A mediolateral oblique view (MLO): For this, the patient stands at a 45° angle to the device. The examined breast is lifted and compressed under tension, while the patient’s upper arm lies on a support in a relaxed position. With the right setting, this offers a full image of the breast parenchyma and the pectoralis muscle up to the nipple, with an angle of at least 20°. The nipple is shown in profile, and the inframammary fold should be visible.
- A cranio-caudal view (CC): The patient stands and turns medially by 10°. The chest is elevated, pulled slightly laterally away from the chest wall, and compressed under tension. With the right setting, this offers an image of the breast parenychma, with the nipple visible in profile. The pectoralis muscle and the axillary part of the gland are also shown in full.
To ensure a high-quality diagnostic mammogram that will lead to reliable breast cancer detection, radiographers should check that the breast is sufficiently compressed. Throughout the process, they should guarantee the patient’s understanding and cooperation. This compression is crucial to sufficiently spread out the glandular tissue to achieve a high-contrast and overlap-free image of all the breast structures.
Step 5: Assessing and classifying the images
In organized screening programs, after the exam, two specialist radiologists independently evaluate the images. If one of them finds something unusual or unclear, a third specialist is consulted.
For early breast cancer detection, it’s important that the diagnostic mammogram is systematically assessed to a set standard. The following process has proven effective:
- Check the quality of the images and make sure they are complete (i.e., adequate compression, symmetrical display of both breasts)
- A systematic search for pathological changes. A side-by-side comparison is vital
- If there are conspicuous findings: assess the size, shape, boundary and shadow density; give a precise localized description of the changes
- Accurately analyze calcifications and microcalcifications by size, shape, distribution and number
- If available: compare with previous images and search for new changes
Next, the findings of the diagnostic mammogram are classified according to BIRADS. However, if possible, a BIRADS level 3 should be avoided in routine mammograms. In unclear cases, it’s better to use a BIRADS level 0 – this means that the patient is offered further screening exams.
It’s best to record the parenchyma density in line with the assessment guidelines set by the American College of Radiology (ACR), as this impacts the quality of the mammogram. Given the age of most patients in these screening programs, glandular tissue will have been replaced by fatty tissue. This lends greater rigor to the results of a diagnostic mammogram.
Step 6: Receiving the mammogram report
Women who take part in diagnostic mammogram screening for breast cancer usually receive the results in the mail within a few days.
In the US, the Mammography Quality Standards Act (MQSA) states that women must receive the results within 30 days of the exam, and that this should be written in a clear and jargon-free way.
Any suspicious or abnormal findings have to be fast-tracked and must include additional information on the next steps. About 97% of women receive normal results and will be asked to have mammograms at routine intervals.
Step 7: Further exam in the case of unclear or suspicious findings
If the findings are unclear or suspicious, the patient is referred to the radiology center for a follow-up exam. If further imaging exams can’t rule out the suspicion of breast cancer after the initial diagnostic mammogram, the next step is a histological examination. This is a minimally invasive procedure, where a vacuum or punch biopsy is done to collect a sample.
Step 8: Further methods for breast cancer diagnosis after a diagnostic mammogram
If the mammogram and further screenings confirm the suspicion of breast cancer, radiologists now face the difficult task of giving the patient comprehensive information and discussing how to proceed. For this appointment, the patient should be advised to bring along someone they trust. Doctors should encourage questions, and offer further help, such as psycho-oncological support. Subsequent treatment should take place at a certified breast cancer center, if possible.
Diagnostic mammograms for early breast cancer detection: Further optimization possibilities
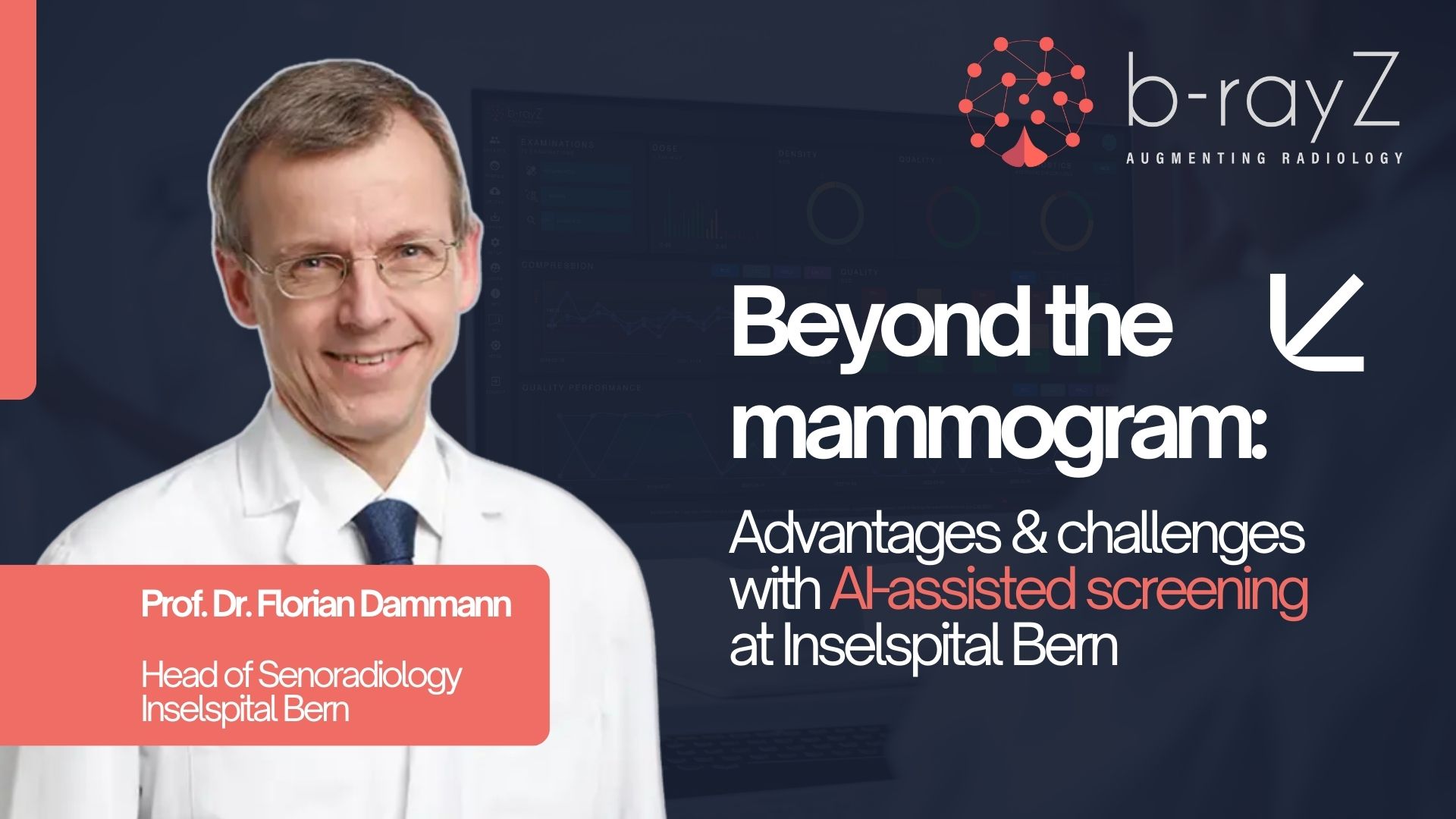
By standardizing and optimizing all the processes in breast cancer detection, this can effectively reduce workloads associated with mammograms without cutting corners in the “wrong” areas of screening programs, such as patient consultations. Doubtless, there is considerable work and effort required in the process. One solution could lie in technologically assisted systems such as artificial intelligence (AI). AI systems are already offering powerful support in the field of diagnostic mammograms, improving process efficiency and leading to more precise diagnoses.